Reinvention and Menopause
Reinvention and Menopause: A Weighty Subject.
Perimenopausal symptoms can vary greatly and last for just months or several years. Every woman is different, but the menopausal symptoms are interconnected and directly influence one another. Women often find that what has worked in the past, will no longer work in the future… and so it may be beneficial to look at this as a time of “reinvention” of both body and spirit. It is a great time to use the wisdom accumulated over the years to adapt at navigating the many changes that come during mid-life. Perimenopause is the physical “change” that mirrors a reflection in time when women find themselves transitioning in many aspects of their lives including career change, children becoming independent, caring for aging parents, and new illness for themselves or their spouse. Women may have put the needs of others in front of their own for decades and now find that pivoting to self-care and creating a supportive system is imperative to their own success.
Weight gain is something that comes up A LOT and being overweight does have inherent health risk.
I often hear women say, “I haven’t changed anything, and I’m gaining weight.” Seemingly overnight, a diet and exercise routine that’s helped you maintain a healthy weight for most of your adult life isn’t working the way it once did. The rules of your body have changed. In perimenopause, maintaining your usual weight can become more difficult. In fact, many women gain weight around the menopause transition. Menopause weight gain is not inevitable, however. Importantly, weight gain can increase risks to your health and should not be ignored.
What causes menopause weight gain?
The hormonal changes of menopause can make you more likely to gain weight around your abdomen than around your hips and thighs. Hormonal changes alone are not the sole culprit of menopause weight gain. Weight gain is often tied to aging, lifestyle, and genetic factors.
For example, muscle mass typically diminishes with age, while fat increases. Losing muscle mass slows the rate at which your body uses calories (metabolism). This can make it more challenging to maintain a healthy weight. If you continue to eat as you always have and don’t build muscle mass or increase activity level… you’re likely to gain weight.
How risky is weight gain after menopause?
There are risks associated with excess weight, especially in the midsection, increases risks of DM, high blood pressure as well as heart disease and both breast and endometrial cancer. You can reverse course by paying attention to healthy-eating habits and leading an active lifestyle.
What’s the best way to prevent weight gain after menopause?
There’s no magic pill. These lifestyle habits are more important as we get older and self-care becomes imperative to our success.

- Exercise. Physical activity, including aerobic exercise and strength training, can help you shed excess pounds and maintain a healthy weight. As you gain muscle, your body burns calories more efficiently — which makes it easier to control your weight.For most healthy women at least 150 minutes a week or vigorous aerobic activity is recommended.In addition, strength training exercises are recommended at least twice a week.
- Nutrition. To maintain your current weight — let alone lose excess pounds — you might need about 200 fewer calories a day less than you did before. To reduce calories without skimping on nutrition, pay attention to what you’re eating and drinking. Choose more fruits, vegetables and whole grains, particularly those that are less processed and contain more fiber. In general, a plant-based diet is healthier than other options. Legumes, nuts, soy, fish are good choices. Anti-inflammatory and antioxidant-rich foods are key. Drink more water daily.
- Stress Management. Ensuring you have intentional time away from stressors and incorporate healthy coping techniques into daily habits.
- Sleep and Mood. Sleep disturbances and mood disorders are critical to manage in the menopausal period and they directly influence weight gain. It is crucial to address these issues to ensure that you are getting adequate and restorative sleep and have the energy level required to create a healthy lifestyle.
- Limit Alcohol Intake. Drinking alcohol can cause weight gain, interfere with sleep, and make menopause symptoms worse.
As women transition into menopause there is a dearth of resources and support available. This is in stark contrast to other stages of a woman’s life. There are a lot of resources and support for new moms, for example. Empowering women to make informed and educated decisions about their health in a space that is both collaborative and supportive is what we are passionate about at Roots Health DPC. Learn more about how we provide health care that is custom tailored to suit your health needs.
Menopause Symptoms
BEYOND HOT FLASHES: MENOPAUSE SYMPTOMS THAT MIGHT SURPRISE YOU
We have all heard about hot flashes and night sweats, but there are more varied and intrusive symptoms that you may not realize are related to perimenopause. Did you know that the fluctuating hormone levels associated with perimenopause and menopause can lead to joint aches, urinary tract infections, changes in your sense of taste, brain fog, and heart palpitations?
Many perimenopausal symptoms can be confused with more serious medical conditions. If you are experiencing any of these symptoms, it is important to speak with your doctor to rule out other causes. Once you and your doctor agree that menopause is the culprit… you can work collaboratively to manage symptoms so you feel your best.
Do you have enough time to get the answers to all of your questions at your visit? Are you looking for a doctor who spends the time listening and really knows what is going on? Does your physician collaborate with you to create a plan that works for you? At Roots Health DPC we believe that spending time with patients is the key to providing excellent medical care. Our visits are unrushed and unlimited. Dr. Diaz is available directly via text and phone to answer the questions that inevitably come up between visits. Schedule a complimentary consultation today.
Menstrual Changes
Classically menopause has been defined as NOT having a period for a year. But during the perimenopausal time, periods can be lighter or heavier and occur more frequently or less frequently than usual. It is important to exclude other causes for irregular periods such as thyroid abnormalities that may be contributing to the picture.
Night Sweats and Hot Flashes
We all know that hot flashes and night sweats are typical perimenopausal symptoms. Estrogen reaches every organ of a woman’s body. Estrogen levels affect the brain and as they drop the thermoregulatory center that controls temperature (hypothalamus) is affected.
Body Image and Weight Gain
As estrogen levels drop, fat distribution begins to shift from the hips and thighs to the abdomen. Weight gain often occurs. During perimenopause, many women experience this increase in visceral fat along with a decrease in muscle mass which studies have shown raises the risk of developing heart disease and diabetes.
Sleep Disruption
Difficulty falling asleep or staying asleep are both common during the menopause transition. Fragmented or poor-quality sleep challenges many women during menopause. Chronic Sleep disruption can be alarming in it’s insidious nature and has many medical and psychological impacts.
Fatigue
Feeling fatigued or exhausted during menopause is common. This can be caused by fluctuating hormone levels, sleep disturbances, or a combination of both.
Sexual Concerns
Decreased estrogen levels leave vaginal tissue less elastic. The tissue becomes thinner and may tear, causing pain during intercourse. In addition, vaginal secretions lessen which means less lubrication. Women may experience decreased libido. This can be multifactorial and go beyond hormonal changes to include body image, stress and life changes, energy levels and a host of other factors.
Neurological Changes
Feeling unfocused and having difficulty concentrating, often called “brain fog,” is a common complaint during menopause. Sometimes brain fog is caused by the sleep disturbances or fatigue that can come with decreasing hormone levels. Estrogen supports memory function, so when it begins to decline, you may feel like you are less able to recall names and other facts.
Musculoskeletal Problems
Some experience body aches, muscle aches, and joint pain. Estrogen helps to reduce the body’s inflammation, and when it declines, joints have less of the natural lubrication that helps them move easily and without pain. Estrogen supports bone strength. Without enough estrogen your risk of osteoporosis increases. Preventing osteoporosis is key and good habits are important to cultivate.
Heart Palpitations
The feeling that your heart is racing, pounding, or fluttering is a sign of heart palpitations. Typical episodes that occur secondary to menopause are usually short lived and harmless and associated with hot flashes.
Changes In Skin, Nails, And Hair
Decreased elasticity in the skin is one of the effects of declining estrogen levels during menopause. Your skin may feel overly dry and more sensitive than usual. Less moisture affects fingernails and toenails. This can leave your nails feeling weak and brittle, and they may break or tear easily. Decreases in the amount of estrogen can also cause hair loss or thinning hair.
Taste Changes
Less moisture in the body affects saliva production. In addition to burning sensations or dry mouth, on occasion women experience changes in how food tastes during menopause. A metallic taste in the mouth can occur.
Urinary Dysfunction
Declining hormone levels can weaken the muscles in the pelvic floor. These muscles control bladder function. The result can be urinary incontinence and women can release urine without warning. Some women can develop urinary tract infections and benefit from treatment.
Education on this stage of life has been inadequate in general. We will discuss tools available to break down and manage these symptoms over the next few weeks. Women do not have to suffer these symptoms alone and they deserve the support of their physician to make informed decisions. Many symptoms can be improved with a combination of lifestyle changes, diet-modifications, and hormonal therapies when indicated. Don’t miss the next “Mondays with your MD”… let us send it you for FREE.
Pharmacy hidden fees
HIDDEN FEES AT THE PHARMACY. WHY IT MAY BE CHEAPER TO NOT TO USE YOUR INSURANCE.
“I used my insurance for birth control pills and my copay was $50. The same medication is available for $11.65 when paid in cash. That’s a difference of $38.3. How can the price be so different?”
Most Americans have insurance that offers coverage on prescription drugs, but not all medications are covered. When your pharmacy collects a copay with your prescription, you can actually end up paying more for the drug than you would have paid in cash.
Why Is My Prescription More Expensive With Insurance?
Depending on your health insurance plan and policy, you may pay more for your medication if your plan requires you to pay a set copayment to the pharmacy for your medication. Regardless of the cost of your medication, you would be responsible for this copayment, but sometimes your copay could be more costly than the medication itself.
Most of us believe that a copayment on prescriptions assumes that the insurer and the patients share the costs of the drug. However, when a copayment exceeds the cost of the medication itself, the prescription benefit manager (PBM) keeps the difference as a profit. A common example would be when you pick up a standard antibiotic or blood pressure medication which cost $4 and your copay is $10.
How Insurance Prescription Coverage Works?
Prescription coverage varies by insurance plan and the list of prescription drugs covered in a health insurance plan is called a formulary. If the medication you have been prescribed is not on the plan’s formulary, you may have to pay for that prescription out-of-pocket.
The cost of your prescriptions may depend on how the costs are factored into your deductible and your actual cost of medication is not known until the prescription is sent to the pharmacy.
Another little-known secret driving up the price of your prescriptions is known as a copay “clawback.” These are prescription drug overpayments that occur when your copayments exceeds the total cost of the drug. The insurance company tells the pharmacy what to charge. The insurance company can overcharge the consumer, forcing the pharmacy to collect that amount, and then takes the extra money back as profit. This practice is carried out through a middleman, known know as a pharmacy benefit manager, or PBM. PBM’s negotiate drug prices with drug companies on behalf of your insurer. Some PBM’s then charge a co-pay that exceeds the cash price.
Nearly half of the insured individuals whose plan doesn’t cover their prescription end up not filling their prescription. Almost one-third of insured individuals across all income groups also said that they or someone in their household was told their insurance plan would not cover a drug prescribed by their doctor.
https://www.healthcaredive.com/news/pbm-practices-consumers-generics-savings-USC/624702/
We’re disrupting the status quo in health care. At Roots Health DPC we believe patients deserve easily accessible health care at an affordable price. We provide excellent medical care and make it easy for patients to get the medications and services they need. Schedule a free consultation with Dr Diaz today and find out how much you can save
How to Save Money on Prescriptions
Consider the following tips to optimize savings on your prescriptions:
1. Opt for the Generic Version
Opting for the generic version instead of the brand-name drug can offer huge savings. Generic medications are the same as brand-name drugs in dosage, safety, strength, route of administration quality, and intended use. The significant difference between brand name and generic is the cost. The price difference out-of-pocket comes down to the patent behind the brand name. Speak to your physician about what your options are.
2. Ask for a Different Medication
Your physician does not know which medications are on your formulary, but it is likely they are familiar with alternative drugs that are used to treat the same condition. If your prescription is not covered by your insurance and requires a hefty out-of-pocket cost, ask your physician what alternatives exist. At Roots Health DPC we help patients obtain medication at affordable prices.
3. Change Your Pharmacy
Surprisingly, the cost of your medication can vary depending on pharmacies. You can try GoodRx for your prescription if you have to pay out-of-pocket and consider changing pharmacies for a better price.
Prediabetes Screening
What is the best way to screen for Prediabetes and What Can I do if I have prediabetes?
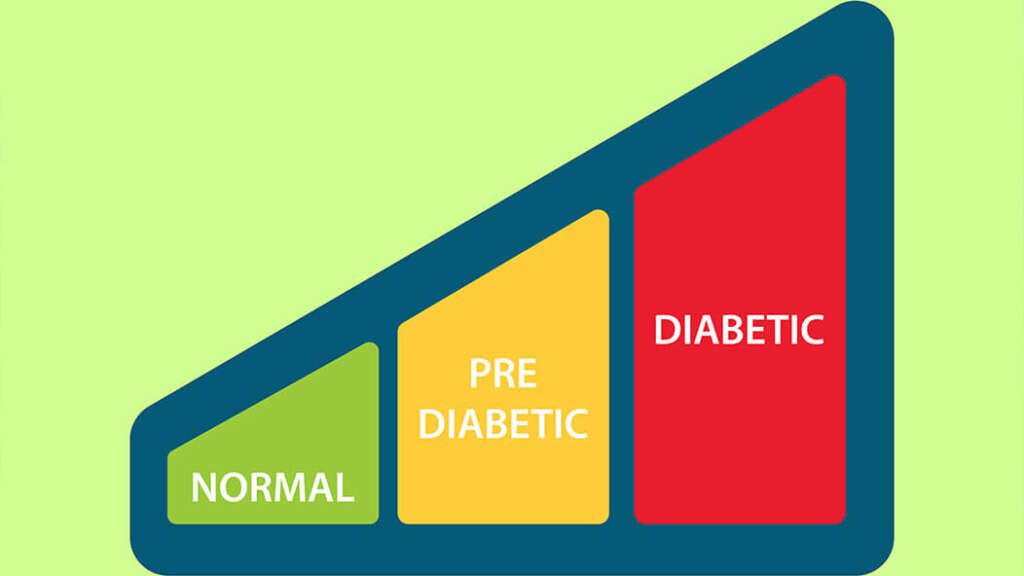
Prediabetes is a diagnosis that gives us the opportunity to avoid developing diabetes and any of the complications that accompany it. I often refer to this as a warning sign… like the red “check-engine” light that comes on when your car needs servicing. Looking at the diagnosis as an opportunity to improve our health can dramatically shift our response to a new diagnosis and the actions we take.
Diagnosis
There are multiple available tests that are used to evaluate for prediabetes and diabetes. If a blood test shows that your blood sugar is higher than normal but not high enough to be called diabetes, it is called “pre-diabetes.” The most commonly used tests are:
- One test measures glucose after fasting.
- Impaired fasting glucose consistent with pre-diabetes is between 100-125 mg/dL.
- Diabetes is diagnosed with a fasting glucose of 126 mg/dL or higher.
- Another test, Hemoglobin A1C, measures how much glucose has attached to red blood cells and provides a view of your blood sugar levels over the past three months. This test does not require fasting.
- An A1C value of 5.7 percent to 6.4 percent is classified as prediabetes.
- An A1C value of 6.5 percent or higher is consistent with diabetes.
What can I do if I have pre-diabetes?
If you have pre-diabetes, you can make lifestyle changes to lower the chance of developing diabetes. Here’s what you can do to prevent Diabetes:
- Eat a healthy diet – Try to eat a diet with lots of fruits, vegetables, and low-fat dairy products, but low in meats, sweets, and refined grains. Basic principles of healthy eating, portion control and counting carbohydrates will serve you well.
- Weight Loss- If you are overweight, trying to get to a healthy body weight can help. Losing 5 to 10 percent of your body weight can lower your risk a lot. Your doctor can help you find healthy ways to do this.
- Physical Activity: be active for 30 minutes a day – You don’t have to go to the gym or do heavy exercise to get a benefit. Activities like walking, gardening, and dancing can all help improve your health.
- Quit smoking – If you smoke, talk to your doctor about how to quit. People are much more likely to succeed if they have help when quitting.
- Consider medical interventions –You might try a medication to lower your chances of developing diabetes, especially if lifestyle changes aren’t helping enough. One drug that is often recommend in these cases for persons with prediabetes is metformin. You can discuss this option with your doctor.
Uncontrolled diabetes is a serious disease with complications that include kidney failure, limb and vision loss. The diagnosis of Prediabetes is an opportunity to change the trajectory of your health and wellness journey. Educate yourself and ensure you are working with a doctor you trust to answer all of your questions, all of the time.
Prediabetes – Signs and Symptoms
What are the Signs of Diabetes? Why should I be screened for Prediabetes if I don’t have any symptoms?
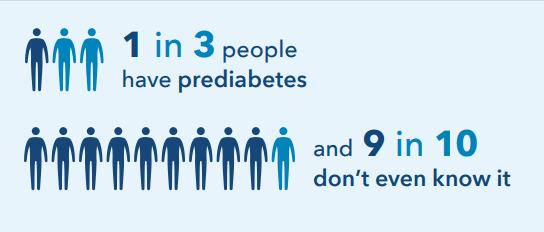
Since 1 in 3 American adults have prediabetes (most of whom do not know they have it) and the risk increases with age… everyone should be tested based on their risk. Middle age is when prediabetes and diabetes diagnoses really begin to spike, but some younger people are at higher risk.
What increases my risk for type 2 diabetes?
There are a few things that can increase your risk of diabetes, these include:
- Being overweight or having obesity, especially if you carry your extra weight in your belly area
- Being 45 years old or older
- Not doing enough physical activity
- Smoking
- History of diabetes during pregnancy, called “gestational diabetes”
- History of polycystic ovary syndrome
- History of high blood pressure
- Family history of diabetes
- African American or Latino
Are there signs & symptoms?
The classic symptoms of DIABETES can include
Excessive thirst
Excessive hunger
Increased frequency in urination
Weight loss
But you can have both DIABETES and PREDIABETES for years without any symptoms
A really important piece for improving your health and wellness is the ease with which you can obtain information from a trustworthy source. Are you able to call your doctor directly and get all your questions answered? If you are looking for a physician who makes it simple to get your health care needs met, schedule your initial free consultation today.
Diagnosing pre-diabetes earlier increases the length of your life. Join us next week to find out how to screen for and diagnose prediabetes.
Prediabetes – What is it exactly?
What is prediabetes? Who is at risk?
A look at the myths about diabetes.
Approximately 96 million American adults—more than 1 in 3—have prediabetes. Of those with prediabetes, more than 80% don’t know they have it. In fact, most people are not aware that they should be routinely screened.
So what is the harm in having prediabetes?
Prediabetes significantly increases the risk of developing type 2 diabetes, heart disease, and stroke. As with anything… knowledge is power.
The good news is that if you have prediabetes, which is easily detected on bloodwork, you can make lifestyle changes to prevent or delay type 2 diabetes and other serious health problems.
Today we are going to dispel some common myths about Diabetes.
Myth: You’re not at risk for Diabetes if you’re a healthy weight
Being obese or overweight is associated with a number of health problems, and it increases your risk for type 2 diabetes. This does not mean that you are immune to the disease if you maintain a healthy weight, however. Even people at a healthy weight can have diabetes
Myth: No One in My Family Has Diabetes, so I Can’t Get It
Having a close family member with type 2 diabetes does put you at increased risk for developing the condition. But the risk of diabetes goes up with age. The risk is higher in people with heart disease, high blood pressure, and who have excess weight or obesity, regardless of family history. Although you might not be able to change your family history or age, you can practice a healthy lifestyle to cut your risk.
Myth: There’s Nothing That You Can Do to Prevent Diabetes
Even though genetics factor into your risk for type 2 diabetes, lifestyle choices play an important role in preventing diabetes. Maintaining a healthy weight, daily exercise and healthy diet modifications can help reduce your risk for diabetes. Smoking can make it difficult for your body to use insulin, so not smoking can help decrease your risk for diabetes, as well. Alcohol consumption can also play a role.
Myth: It’s Your Fault if you have Diabetes
Diabetes is a serious chronic disease, and people with diabetes are not to blame. There is no known way to prevent type 1 diabetes, and while lifestyle factors do contribute to your risk for type 2 diabetes, even type 2 diabetes is not entirely preventable.
Myth: Diabetes is Inconvenient but not Serious
Diabetes results in more deaths than breast cancer and AIDS put together. There are several risks and complications associated with diabetes, including heart disease, stroke, blindness, kidney failure, and lower limb amputation that impact the quality of life significantly.
Making Health Your Priority in 2023: Tips for Success
The goal of becoming healthier is among the most popular resolutions. Many resolve to eat healthier and exercise regularly. These resolutions are great, but they do not address the way stress can sabotage our best efforts to live a healthy life. Emotional well-being underpins our success at achieving our health goals for 2023.
Goal setting is good, but the mindset work that builds the foundation for the path to success is what is most important. Living a healthy life is a journey, not a destination, and there are no “quick cures” when it comes to health and well-being. Failure can cause impatience and it is necessary to remember that you will succeed… if you don’t expect overnight success.

Use these tips to help ensure you follow through with prioritizing your health in 2023:
Stay in Touch
Connect with friends in person. It’s good for your health to maintain friendships. In general, a lack of social bonds can damage your health as much smoking, obesity, and high blood pressure.
Surround yourself with people who are making their personal health and wellness their priority. In a technology-fixated era, it’s never been easier to stay in touch, so fire up your favorite social media and then follow up with in-person visits.
Plan for bumps in the road: A support system can help. We thrive with social interaction and support. Surround yourself with like-minded people looking to prioritize their health and wellness this year. It is important to have someone there on a regular basis to get you through those rough times.
Manage Your Stress
Stress, in small doses, can actually be helpful for short periods. But chronic stress can increase your risk of—or worsen—anxiety, depression, diabetes, heart disease, and more. The best way to manage stress is to control the factors you have agency over:
- Get enough sleep
- Exercise
- Ensure you are eating well
- Spend intentional time relaxing away from stressors
Relaxation, sleep, socializing, and taking vacations are things we all deserve and owe to ourselves for our health and well being in 2023. Finding healthy ways to cope with the stress in your life is imperative to your well-being.
Cut Back on Alcohol
Drinking alcohol in excess can increase risk for depression, increase memory loss, and increase hot flash symptoms in perimenopausal women. Heavy chronic drinking increases your risk for liver and heart disease, stroke, mental deterioration, and even cancers of the mouth, throat, liver, and breast.
If cutting back on alcohol to a couple of drinks per week seems to be difficult, consider reaching out for help.
Get More Sleep
You probably already know that a good night’s rest can do wonders for your ability to function on all cylinders. But sleep is more beneficial to your health than you might realize. A lack of sleep has been linked to a greater risk of obesity and type 2 diabetes.
Aim to get quality sleep and more of it by exercising good sleep habits. These habits can include actions such as:
- Going to bed and waking up at consistent times daily
- Having a comfortable bedroom atmosphere (i.e., one that is dark, quiet, and relaxing)
- Getting exercise during the day
It’s common for people to make New Year’s resolutions, but it’s also common for people to break them. Fortunately, there are resolutions you can make with ways that can help you stick to them. At Roots Health DPC, we take the time to understand your unique health goals and work with you to address obstacles to your success. We invite you to join us and let us help you achieve your health and wellness goals in 2023.
My Child is Sick… When Should I Be Concerned?
My child has a “virus” but is not getting better… What now?
Hey Moms… we know this winter has been rough. Give yourself and your family the gift of peace of mind around all health related concerns. My patients just call or text DIRECTLY to my cell whenever they have a question. I take the time to understand their concerns and answer all of their questions. Every time.
I was told it is “a virus”…. What should my child be tested for?

Sometimes… The fever is not caused by a virus at all…
If your child has a high fever with a sore throat without a cough… you likely will get a strep test to ensure there is no strep throat.
My child is not getting better… when should I be concerned?
The course of any viral illnesses can last 1-2 weeks. Fevers can usually be controlled with medication, like Children’s Tylenol, when given in the correct dose. Fevers generally resolve within 5 days. The cough may linger around for a while afterwards.
Children who have had recent viral upper respiratory infections are at greater risk for developing a secondary bacterial infection. Generally, these occur when the cold is clearing up and the child is improving.
If your child develops a high fever at the tail-end of a “cold” or a worsening cough… then it might be time to take that kiddo in for another exam. Typical bacterial infections that occur at the end of a viral upper respiratory illness can include ear infections and pneumonia. These infections generally occur after the immune system has been weakened by the viral illness.
Signs that may warrant further evaluation with your doctor
- Persistent fever 102 for more than 2 days /recurring/not controlled with medication
- Fever that is above 104 at any time
- Child looks very ill or drowsy or is not consolable
- Signs of dehydration (dry diapers/not peeing, dry mouth and lips despite giving pedialyte)
- Unusual rash
- Very sore throat, bad headache or vomiting
- Has a weakened immune system (children with underlying chronic conditions)
Holiday Stress – Mondays With your MD
Prioritize your mental health this holiday season
‘Tis the season of giving!
Make sure you fill your own cup first…there is nothing to give from an empty cup.
Don’t let stress and negative thinking ruin your holidays and hurt your health.
With some practical tips, you can minimize the stress that accompanies the holidays. Heck…you may even end up enjoying the holidays more than you thought you would!

5 Tips to “enjoy more and stress less” this holiday season:
1. LOWER YOUR EXPECTATIONS
… for yourself and others! The holidays do not have to be perfect… or even just like last year. Families change and grow and so do traditions and rituals. Remember feelings are not facts and they do not last forever. Try to focus on what really matters most to you this holiday season. Acknowledge your feelings and give yourself the space and time to process them and then, when you’re ready, choose to move on.
2. KEEP YOUR ROUTINE AND HEALTHY HABITS
Don’t let the holidays become a free-for-all. Overindulgence only adds to stress.
- Get sleep
- Eat healthy meals
- Avoid excessive alcohol
- Include regular physical activity
- Use deep-breathing exercises, meditation or yoga.
3. PRACTICE MORE SELF-CARE
Make time for yourself and take a break. Reserve spending time just for you, without distractions. Engage in hobbies that bring you joy: take a walk, enjoy music, listen to an audiobook, get a massage, let your artistic side play. This simple tip may refresh you enough to handle everything you need to do.
“You should sit in meditation for 20 minutes a day, unless you’re too busy: then you should sit for an hour” –old Zen proverb
4. SAYING “NO”
Saying yes when you should say no can leave you feeling resentful and overwhelmed. Friends, family, and colleagues will understand if you can’t participate in every activity or if you are unable to host them beyond your limits. Remember that “No” is a complete sentence. If you have an obligation that is taking more time than planned, try to remove something else from your agenda to make up for the lost time.
5. ASK FOR HELP
Reaching out for help during the holidays is one of the best things you can do. Speak with a person you trust…a friend, family member or your therapist, about your current feelings. You will discover that feeling down or stressed during the holiday season is very common. Give yourself the time you need to use tools to overcome those negative thoughts. Seek professional help if you need it. Despite your best efforts, if you find yourself feeling persistently sad or anxious, plagued by physical complaints, unable to sleep, irritable and hopeless, and unable to face routine chores… talk to your doctor or mental health professional. You are never alone.

YOUR TIME is valuable – Mondays with your MD
YOUR TIME is the most valuable resource you have. Give yourself the gift of TIME.
You work hard to balance time between your career and your family. When one of your own has a health concern that “pops up” or just needs to be scheduled …. trying to figure out the how, where, and when to get the issue addressed can literally take hours, and even days, from your routine.
I get it. I’m a working mom and I know what it is like to balance work and family, to “carry” the mental load, and then…. to put “one more thing” on your plate. My job is to take that stress off your plate.
“My son has a sore throat and fever…. I have placed a call to his doctor’s office and am waiting for a call back….”
When you have medical concerns, the last thing you want is to pile on more stress. Let me help! My patients reach out to me, their physician, directly via text at any time of day. They get answers to the questions they have about their health immediately and can take the next steps and get back to their busy lives.
“My daughter cut open her foot. Do I take her to urgent care or ER and wait to be seen?”
No one has time to wait around for a return call from the doctor’s office for advice. You don’t have to sit in an urgent care with other contagious sick people waiting to be seen… then go back again the following week because you picked up a virus in the lobby while waiting. We take care of this without the wait!
“I am experiencing a constant feeling of being tired… but I just put off going to see the doctor because it is so hard to get an appointment and the visit takes up half my day.”
Let us make going to the doctor as easy as booking a time that works perfectly for your schedule. We even offer telemedicine so you can get care wherever you are. If you are visiting us, there is no waiting in a waiting room. Ever!
THIS IS NOT too good to be true!

Ditch the Healthcare Hassle. Give yourself the gift of Time!
Get all the health care needs for your family met with ease and grace. We know how valuable your time is and that is why we are making health care easy for families: one mom at a time.
Come and see how Direct Primary Care works….schedule a free initial consultation with us today and get all your questions answered.
YOU DESERVE BETTER CARE
What is a Sinus Infection? – Mondays with your MD
This cold and flu season, I am getting a lot of questions about sinus infections.
So today, we are reviewing which treatments work best.
What is a sinus infection?
The sinuses, air-filled pockets in bones of the face, form the top part of the respiratory tract. A sinus infection occurs when the tissue in the sinuses swells and leads to a buildup of mucus, pain, and discomfort.
Viruses cause 9 out of 10 sinus infections in adults. Here we discuss symptoms and treatment options for Viral Sinus Infections.
Common symptoms:
Pain or pressure in your sinuses
Facial pain is a common symptom of sinusitis. You have several different sinuses above and below your eyes, as well as behind your nose. Any of these air-filled cavities can hurt when you have a sinus infection. You may feel pain in your forehead, on either side of your nose, in your upper jaws and teeth, or between your eyes
Tenderness in the face
Your face may also be tender to the touch due to the built-up pressure. This tends to occur at the bridge of the nose or under the eyes, and can occur on the forehead and cheeks.
Runny nose and postnasal drip
When you have a sinus infection, you may need to blow your nose often because of nasal discharge. This discharge comes from your infected sinuses and drains into your nasal passages. The discharge may also bypass your nose and drain down the back of your throat causing irritation or sore throat. This is called postnasal drip, and it may cause you to cough. It can also cause your voice to sound hoarse.
Sinus headaches
Persistent pressure and swelling in your sinuses can give you symptoms of a headache. Sinus pain can also cause earaches and pain in your teeth, jaws, and cheeks. Sinus headaches are often at their worst in the morning because fluids have been collecting all night long.

What can I do?
Most cases of acute sinusitis get better on their own. Self-care techniques are usually all you need to ease symptoms. In general, antibiotics are not needed and do not help symptoms (as it is usually caused by a virus anyway).
Consider the following options:
1. Pain medication
Over the counter anti-inflammatory medications such as ibuprofen can provide relief of headache, facial pain, and sore throat if they are not contraindicated.
2. Intranasal steroid sprays
These reduce inflammation and decrease swelling in nasal passages. This can be particularly helpful for patients with allergic symptoms as well. Commonly we use fluticasone nasal spray.
3. Decongestants
These are typically Pseudophedrine or Phenylephrine. They can relieve congestion and pressure but may cause a rebound effect when stopped. There are contraindications for some patients with high blood pressure and other risks.
4. Nasal Irrigation
Using a neti pot with sterile intranasal saline is highly recommended for most. These generally provide safe and effective temporary relief.
Signs that you should seek care
Consult your doctor if you have:
- a high persistent fever (>102F)
- symptoms that have lasted for more than 10 days
- symptoms that are getting worse
Mondays with your MD – Not another respiratory virus…. It SNOT FUNNY!
Winter is coming….. that means LOTS of colds/flu…. AND its WORSE than ever before ALREADY! This is the first fall with our masks off…. And all these infections are coming back out with a vengeance.
The kids are coming home from school and everyone needs more tests and notes to return to school and work than ever before. As a working parent…. I know your time is valuable… you need the highest quality and fastest care possible.
No one wants to go to an urgent care with a bunch of other sick people and pick up another virus to deal with in the home next week!
Its not a surprise that after the disappearance of COVID mitigation strategies and low population immunity, as kids have flocked back to classrooms and day cares, there is a huge upswing of respiratory viruses circulating. RSV, rhinovirus, flu, Covid… you name it. Children, on the whole, are more susceptible to these microbes then they have been in years.
Most of these viruses have been around forever and many have always posed a risk for infants/toddlers, patients with underlying respiratory diseases and immunocompromised folks. This year, flu, covid, and other commonly known respiratory viruses including RSV are on the rise to the highest levels seen in decades.

Ways to prepare for THIS cold and flu season…
Get your flu shot and COVID boosters NOW if you have not already.
Wash your hands and kids hands frequently. Use hand sanitizer to avoid germs
Avoid areas with other people with cough and cold symptoms
Breastfeed: it transfers immunity to babies to fight infections
Eat healthy with plenty of fresh fruits and vegetables.
Stay rested. Getting sleep helps your immune system stay strong

If you want to know the most effective upper respiratory infection treatments and learn how to navigate this winter to minimize the disruptions to your routine …… sign up for our FREE GUIDE to
“Best practices for the common cold, flu, and COVID”
If you want to know the most effective upper respiratory infection treatments and learn how to navigate this winter to minimize the disruptions to your routine …… sign up for our FREE GUIDE to
“Best practices for the common cold, flu, and COVID”
Mondays with your MD – Open Enrollment is Here
The THINGS you DID NOT EVEN THINK to consider this Open Enrollment…..
How can I keep my costs low AND receive high quality accessible health care?
Every year we pay more for insurance while less and less is covered. When we attempt to use our insurance it is cumbersome and inconvenient at best. We have all experienced the frustration with the amount of time it requires to obtain what we need for our health and get it covered by insurance. Today we cover the basics and empower you to make decisions that will give you the most cost-effective way to obtain the high quality health care you deserve
The Jargon
Premium: the amount you pay every month for health insurance.
Deductible: the amount you must pay before you can get any services covered by your insurance in a calendar year. A few Caveats to the deductible: Not everything counts towards your deductible. Premiums and copays generally don’t count. Some plans have separate deductibles for prescriptions.
Copay: a fixed amount you pay for a covered expense (visits, procedures, medications, etc)
Out-of-pocket maximum: the most you might have to spend for covered services in a given year. This number is important to understand!
HDHP is a High-deductible Health Plan (HDHP): these plans offer lower monthly premiums and allow you qualify for a Health Savings Account (HSA)
HSA is a Health Savings Account: A type of savings account that lets you set aside money on a pre-tax basis to pay for qualified medical expenses.
Health Share Plans*: this is not an insurance product and offers much lower monthly premiums with low initial unshareable amount (similar to a deductible). *A cooperative where members “share” medical costs. They cover catastrophic needs (hospital stay, surgery, ER visit, etc) but are not insurance products.

What your typical open enrollment conversation is missing!!!
Smart consumers determine their out of pocket projected cost for the year and choose a high deductible plan to save on monthly premiums. Savvy consumers understand the relationship between premiums and deductibles and keep costs low by determining the most cost-effective way to lower their out of pocket-expenses over the course of the entire year.
REMEMBER HEALTH CARE DOES NOT NEED TO BE EXPENSIVE.
Direct Primary Care: The impossible Made Simple and Transparent.
Direct Primary Care (DPC) removes insurance companies from the physician-patient relationship and provides the vast majority of health care services through a low monthly fee (like a gym membership). Patients skip the hassle of traditional insurance-based care. They get more time with their physician with same day and next day appointments… all without copays or hidden fees. DPC can produce tremendous savings on out of pocket expenses when patients work with their DPC physician to find the most cost-effective appropriate health care. The enormous savings on medications, labs, and imaging often exceed the annual cost of membership.
Can you imagine if you could have easily accessible high quality health care with access to your doctor whenever you needed it AND pay less out of pocket? Have a cough and fever but dont want to go to the urgent care? ….. skip the line and the copay! Urinary tract infection while on vacation out of state?…. no problem we got you covered.
M.C. saved 97% on her bloodwork.
Imagine getting 97% OFF… you read that right! This patient had labs with Roots Health DPC and paid $29.57. The same patient had the exact same labs billed (for the same tests) at a price of $901.24 through the same lab.
At Roots Health DPC we get it. Your health and wellness are our main goal and we are here to support our patients as they make decisions that will affect their well-being.
Open enrollment only comes once per year… make the most of it and choose the best plan to meet your health care needs.
Its your money.
Its your healthcare.
Its your choice.
If you want to learn more about how direct primary care can help you achieve your health care goals and save you money, sign up for our free guide:
“Better Healthcare for a Fraction of the Price”
If you want to learn more about how direct primary care can help you achieve your health care goals and save you money, sign up for our free guide:
“Better Healthcare for a Fraction of the Price”
Mondays with your MD – Breast Cancer Warning Signs (Part 3)
The 5 signs of Breast Cancer
Breast Cancer Screening is for women without symptoms. However, if you notice
any symptoms of breast cancer you should see your doctor for an evaluation
promptly regardless of when you were last screened.
The warning signs of Breast Cancer
1. If you notice a lump that feels firm or fixed in the breast or underarm area
2. Swelling, warmth, redness or darkening of the breast skin
3. Change in the size or shape of the breast including dimpling or puckering of skin
4. Nipple retraction or change in position of nipple
5. Discharge from your nipple
Although the vast majority of breast cancers are found through abnormal mammograms, up to 30% of breast cancer patients present with a mass that occurs between mammograms.
This is part THREE of a THREE part series on Breast Cancer Awareness.
Read more here
Part One – Prevention
Part Two – Screening
Never miss another “Mondays with your MD!”
Sign up below
This is part THREE of a THREE part series on Breast Cancer Awareness.
Read more here
Part One – Prevention
Part Two – Screening
Never miss another “Mondays with your MD!”
Sign up below
Mondays with your MD – Breast Cancer Screening (Part 2)
Breast Cancer Awareness Month – Part II: Screening
On average, one out of eight women will be diagnosed with breast cancer. Do you know which screening test is best and when to start screening for breast cancer?
There is more than one type of screening test for breast cancer and there are varying recommendations from different organizations. Education with individualized planning (based on your personal risk for breast cancer) can help determine the best screening test for you.

Mammography is the most common screening test for breast cancer
A mammogram is a low-dose X-ray of your breasts and can find cancer early.
Different experts have varying advice for when to initiate screening and how frequently to screen average-risk women ages 40 to 49. All experts agree that at a minimum screening should occur at least every 2 years between ages of 50-74.
For average-risk women screening mammography can be performed every one to two years based on patient preference.
Magnetic resonance imaging (MRI) may be used to screen women who have a high risk of breast cancer
MRI is a procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. MRI does not use any x-rays and there is no exposure to radiation.
For women with moderately increased risk factors (based on breast density, reproductive history, and hormonal history), breast ultrasound in conjunction with mammogram or a MRI can be considered on an individual basis.
Use of MRI for supplemental screening in women with dense breast tissue has shown higher rates of detection, but there is no evidence that health outcomes are improved overall.
Women with high risk factors (based on a history of chest radiation, ancestry, genes and genetic conditions) may benefit from more frequent screening with enhanced modalities. Obtaining annual MRI and/or consultation to consider risk reduction treatment and intensification of surveillance are viable options.
It is clear that the type and timing of breast cancer screening is highly personalized. You should discuss your risk factors with your board-certified physician so that you can make an informed decision about breast cancer screening.
This is part TWO of a THREE part series on Breast Cancer Awareness.
Never miss another “Mondays with your MD!”
Sign up below
Never miss another “Mondays with your MD!”
Sign up below
Mondays with your MD – Breast Cancer Awareness Month!
October is Breast Cancer Awareness Month
Many of us have been touched by breast cancer- perhaps through a personal diagnosis- or by a family member, friend, or colleague diagnosed with this disease. Breast cancer, after all, is the most frequently diagnosed cancer and leading cause of cancer death in women. Please join me over the next few Mondays to discuss prevention, screening, and warning signs.

Education is Key for Prevention
Do you know the risk factors associated with an INCREASED risk for breast cancer?
- Hormonal factors can influence your risk for breast cancer. Higher levels of endogenous estrogen and hormonal combined estrogen/progesterone replacement has been associated with increased risk of developing breast cancer.
- Reproductive factors associated with a higher breast cancer risk include earlier onset of menstruation, not giving birth or having first child later in life, and a late menopause.
- Family history and genetic mutations. The risk of breast cancer is affected by the number of first-degree female relatives diagnosed with breast cancer and the age at which they were diagnosed.
- The highest breast cancer risk occurs among White women (although it remains he most common cancer among women of every major ethnic/racial group).
- Alcohol consumption is associated with a higher risk of breast cancer.
- A higher BMI in postmenopausal women is associated with increased risk for breast cancer.
Do you know how to DECREASE your risk for breast cancer?
- Breastfeeding. For every 12 months of breastfeeding there is an approximate 4% reduction in the relative risk of breast cancer.
- Increased physical activity at all ages lowers risk.
- Dietary factors may modify breast cancer risk although data is limited. Eating a low-fat high fiber diet with plenty of fruits and vegetables is recommended.
This is part ONE of a THREE part series on Breast Cancer Awareness. STAY TUNED. Next week we will review breast cancer screening options and recommendations.
Want to make sure you don’t miss the next “Mondays with your MD?” Tell me where to send it to you!
This is part ONE of a THREE part series on Breast Cancer Awareness. STAY TUNED. Next week we will review breast cancer screening options and recommendations.
Want to make sure you don’t miss the next “Mondays with your MD?” Tell me where to send it to you!
Mondays with your MD – 5 tips to prevent eczema flares
Winter is coming… 5 tips to prevent eczema flares!
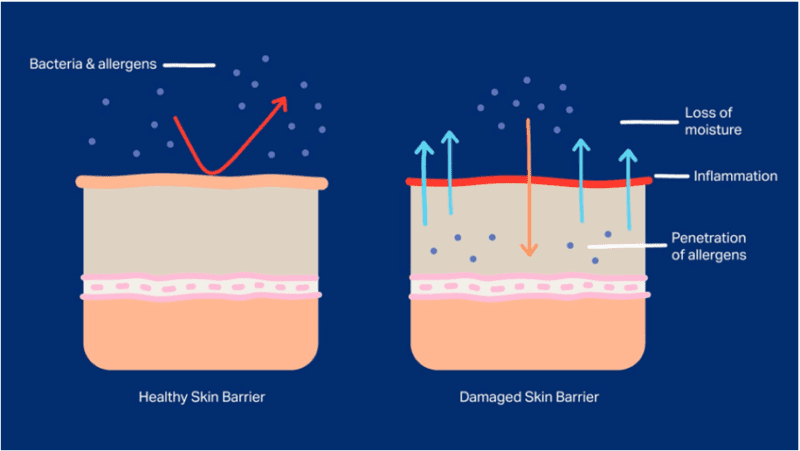
Did you know that your skin is the largest organ of your body? Your skin works as a barrier to prevent infection. When your skin barrier is weakened you experience dryness, irritation, and inflammation. These are all signs that your skin needs attention. Follow these 5 tips to avoid flare-ups….
Keep Skin Moisturized
Moisturizing is key and it must be fragrance free! Slather on gentle, fragrance-free moisturizer several times a day, especially right after bath/shower. Highly recommended brands include CeraVe and Aquaphor.
Avoid Irritants
Highly sensitive skin is prone to irritation with perfumes, dyes, and chemicals found in everyday household products. The trick is to use hypoallergenic and fragrance-free products. Minimize flare-ups and itching by using fragrance-free soaps, shampoos, and detergents.
Be Temperature Aware
Pay attention to temperature and humidity. Take shorter baths with luke-warm temperature water. Avoid exposure to extreme heat/cold and wear 100% cotton allowing skin to breath. This helps with overheating and excessive sweating which can trigger a flare-up.
Supplement with Vitamin D
Vitamin D supplementation and direct sun exposure can lessen the severity of eczema symptoms and support your skin barrier and immune system. Vitamin D supplementation is a safe and tolerable therapy.
Partner with your physician
With eczema-friendly skin care and trigger management most people can control eczema. Your physician can create custom-tailored treatment plans that can include topical medications, specialized dressings, oral medications, or UV light therapy each of which has unique risks/benefits.
Mondays with your MD – Getting to the root of your healthcare concerns
Are you frustrated with the existing health care system? Is your doctor treating your individual symptoms but not helping you find the root cause for the constellation of symptoms you have? Are you wondering if your health care needs might require an integrative approach?
Roots Health DPC provides a patient-centered approach that engages the whole person; nourishes the mind, body, and spirit; and encourages the conscious creation of personal health and wellness. Patients have constant direct access to board-certified medical care with ample time to fully evaluate and treat the root cause of symptoms.
Did you know that the average length of time spent in an office visit to cover patient concerns and circumstances is 7 minutes in the traditional insurance-based health care model? That’s right… 7 minutes! It is no small wonder that the typical health care experience feels piecemeal and rushed. You would not expect your mechanic to diagnose, let alone treat, your car problem in 7 minutes…. so why do we accept this substandard care for our own health and well-being?
At Roots Health DPC, we know that your health is the most important thing. It is the foundation for living life on your terms.

Why should you consider direct primary care for your health care?
Quality time
Quality time to understand your health care needs with your physician and create an individualized health care plan. We focus on the whole patient as a unique individual –taking into account each element of a person’s health, environment, and lifestyle.
Communication
Communication with your board-certified physician that is easy and ongoing making it simple to adjust the plan as necessary to meet your health care needs. Unlimited physician access and visits… in office and virtual
No Waiting. No Copays. Ever.
Affordable Transparent Pricing.
A low monthly membership fee provides unlimited direct access to your physician to work with you as a team to obtain and maintain your optimal health and well-being. Steep discounts on labs, medications, supplements, and imaging.
Sign up here to make sure you never miss a “Mondays with your MD” post
Mondays With your MD – New Covid Vaccine: Bivalent Boosters
The new bivalent booster offers better protection against recently circulating COVID-19 variants and helps restore waning protection from previous vaccination. It offers broader protection for new variants. People must complete the primary series (original monovalent vaccines) before getting a bivalent booster dose.
Who should get the new booster?
- People 12 years and older should receive the updated Pfizer or Moderna (bivalent booster)
This includes people who have received all primary series doses and people who have received the original (monovalent) boosters - At this time children ages 12-17 years can only receive the updated Pfizer bivalent booster.
- Children under 12 years do not get a bivalent booster yet.
What is considered “Up to Date” with all these boosters?
Once you have completed the covid-19 vaccine primary series and received he most recent booster dose that is recommended
When should I get the new booster? Which brand should I get?
The new bivalent booster can be given at least 2 months or more after your last COVID vaccine. The monovalent booster should no longer be given to anyone 12 years of age and older.
It is fine to get a booster from a different brand than the primary series or previous boosters. For example, if your primary series was Moderna you can get the Pfizer bivalent booster.
What about kids under 12 years old?
At this time, children under 12 years old will NOT receive the new bivalent booster dose although this is likely to change in the future.
Children 5 years – 11 years who received Pfizer for their primary series should still get a monovalent booster 5 months after the last dose of the primary series.
Children 5 years – 11 years who got Moderna for their primary series do not get a booster at this time.
Children 6 months – 4 years should get all COVID-19 vaccination primary series doses.
Sign up here to make sure you never miss a “Mondays with your MD” post
Mondays with your MD – Covid … Again? What you need to know
There seem to be more cases of COVID circulating in our community now… so I thought I would share the most common questions and concerns I hear from patients.

My family member has COVID. How often do I need to test myself?
- If you develop symptoms it is recommended to test immediately.
- If you have symptoms and your rapid test is negative it is recommended you obtain a PCR test.
- If you do not have symptoms, you should wait at least 5 days after your exposure to do testing.
- If you are vaccinated and do not have symptoms you do not need to isolate before testing.
Can I really get COVID again? I already had it.
Yes. Everyone 12 years of age and older can receive an updated COVID booster which targets the new COVID variants. Although your disease may not be as severe, you can still catch COVID and pass it to others who may be more vulnerable.
My COVID test is positive… still.
Some patients believe they need a negative test to return to work. The truth is that once you have a positive test there is no reason to repeat a test. The isolation period is 5 days and can last up to 10 days depending on the severity of your illness. If your isolation ends on day 5, you should intentionally wear a mask whenever you go in public until the full 10 days has elapsed.
What is Paxlovid and does it work?
Paxlovid is one of the medications used to treat COVID. It is highly recommended for those at risk for disease progression and it significantly decreases the severity of the disease. Do not delay seeking care as this treatment must be started within days of when you first develop symptoms to be effective.
When you have questions about urgent health concerns, you want accessible advice from your physician. Wouldn’t it be great if you could just text your doctor and ask? At Roots Health DPC that is how we provide medical care! We are available to our patients by phone, email, and text anytime. Schedule a FREE “Meet and Greet” at Roots Health DPC to find out more.
We are now accepting new patients and would love the privilege of serving you in our clinic.