Skin Cancer
Tips for Early Detection of Skin Cancer
What are the skin changes you should not ignore? Skin cancer is the most common form of cancer in the United States. Knowing how to do a skin self-exam and what the warning signs are for melanoma are the key for decreasing risk.
Follow these tips to increase your chances of spotting skin cancer early, when it’s most treatable.
How to perform a skin self-exam
- Examine your body in a full-length mirror– Examine your body front and back in a mirror, then look at the right and left sides with your arms raised.
- Look at your underarms, forearms, and palms– Bend your elbows and look carefully at your forearms, underarms, and palms.
- Look at your legs, between toes, and soles of your feet- Look at the backs of your legs and feet, the spaces between your toes, and the soles of your feet.
- Use a hand mirror to examine your neck and scalp- Examine the back of your neck and scalp with a hand mirror. Part your hair for a closer look at your scalp.
- Use a hand mirror to check your back and buttocks- Finally, check your back and buttocks with a hand mirror.
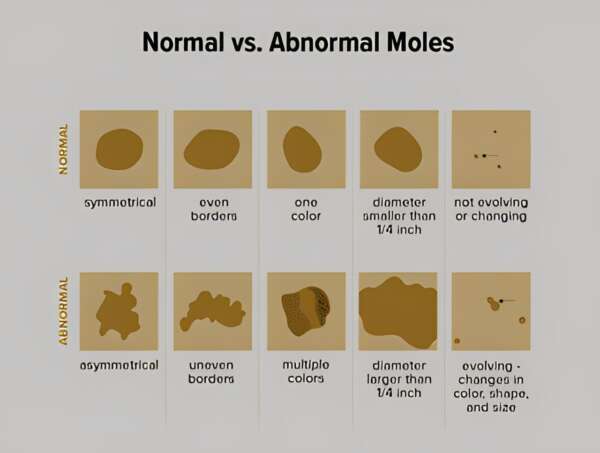
Remember the “ABCDE rule”
Note changes in moles or birthmarks that can be warning signs of melanoma, the deadliest form of skin cancer.
A- Asymmetry where one half looks different from the other
B- Borders of the mole that are irregular or not sharply demarcated
C- Color is varied from one area to another
D- Diameter over 6mm (the size of a pencil eraser)
E- Evolving or changing in size shape or color