Retinoids: Your Skin Care Essential
Skin Care Routines: The Lowdown on Retinoids
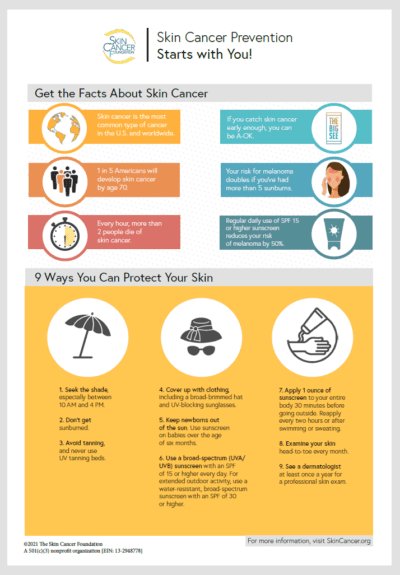
As we age, collagen production slows… causing wrinkles and signs of aging. Eating a diet rich in anti-oxidants, staying hydrated, using daily facial sunscreen and moisturizer are all critical components for a healthy skin care routine. Today we look at retinoids as a basic foundation for anti-aging skin care routines.
What are retinoids?
A derivative of vitamin A, retinoids can tackle everything from fine lines and pigmentation to acne. They achieve this by boosting the turnover rate of skin cells. Retinoids accelerate the rate of skin cell division and new cell growth which helps thicken the top layer. Retinols and other retinoids also work deep in the skin’s dermis layer to stimulate collagen and elastin production. These skin proteins naturally decrease with time, leading to thinning skin and other visible signs of aging. Boosting their production, then, allows retinoids to offer pro-aging support.
What’s Retinol?
When it comes to retinol and retinoids, plenty of people get a little confused — but with good reason. These two anti-aging ingredients aren’t entirely different. In fact, retinol is a sub-type of retinoid.
From reducing the appearance of wrinkles to easing the effects of sun damage retinoids can offer plenty of skin benefits. Retinoids most often describe more powerful prescription products, while retinol generally refers to weaker over-the-counter (OTC) formulas. OTC formulas tend to be less drying but they are still effective… if used consistently over long periods of time.

Should you use retinoid or retinol?
Before deciding, you’ll want to consider your skin type and the severity of the problem you’re trying to treat. Retinols are generally recommended for dry skin as they tend to be less drying and often are formulated with hydration ingredients.
Side effects of retinoids including irritation, redness, burning suggest an overly aggressive routine and can occur if you do not “ease your way” into retinoid use by starting slowly.
Contraindications to all retinoids include pregnancy, lactating, or trying to conceive.
How to use retinoids?
WHEN to put them into your skin care routine: at night after washing with a gentle cleanser. Start 3 nights per week and increase to daily after a few weeks if your skin can tolerate.
HOW to apply: use a pea-size amount when face is dry. Apply moisturizer afterward to avoid irritation. Using sunscreen on a daily basis is a MUST while applying retinoids.
ANYTHING ELSE? Check the ingredient list of your other skin care products, as retinoids can interact with other formulas and should not be used with benzoyl peroxide for example.
Combining retinoids with ethyl alcohol or acidic products, can dry out your skin and lead to redness and irritation.
If you have dry skin, creamier formulas can offer more hydration. If you have normal, oily, or combination skin, you might prefer a thinner gel consistency.