Mental Health Awareness Month
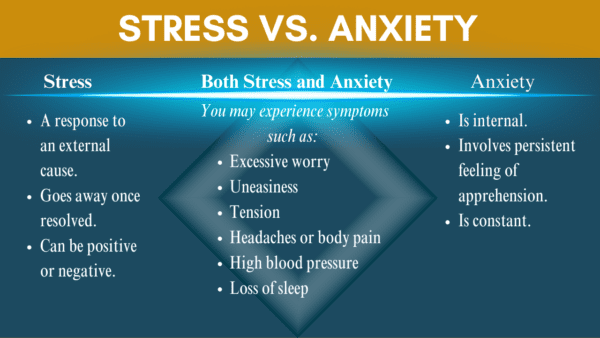
Is It Stress or Anxiety?
Mental Health Awareness Month
Everyone experiences stress, and sometimes that stress can feel overwhelming.
You may be at risk for an anxiety disorder if it feels like you can’t manage the stress and if the symptoms of your stress:
– Interfere with your everyday life.
– Cause you to avoid doing things.
– Seem to be always present.
Practice Self-Care for your Mental Health: Build a toolbox full of healthy ways to cope
Simple, everyday actions:
–schedule quiet time for meditation, yoga, or reading
–spend a few minutes in nature, getting out to exercise, or playing a favorite song can help you feel grounded
–stick to a sleep routine to ensure enough sleep
–keep a journal
–connect with others in your community