EVERYTHING YOU NEED TO KNOW TO KEEP YOURSELF AND YOUR LOVED ONES SAFE
We all want quick COVID test results, understandably. But what we need are accurate results. The worst-case scenario for my patients would be a false sense of security from a negative test when they, in fact, have COVID-19 and could harm the ones they love. This is why public education around testing and results is so important.
At Roots Health DPC, we are committed to sharing information about COVID testing so that you can make informed decisions regarding testing and results. Not all tests are created equal. Below, we review what tests are used to detect whether someone has an active COVID infection, when additional testing might be necessary, and best practices for our patients when it comes to “rapid testing.”
Types of COVID-19 Testing:
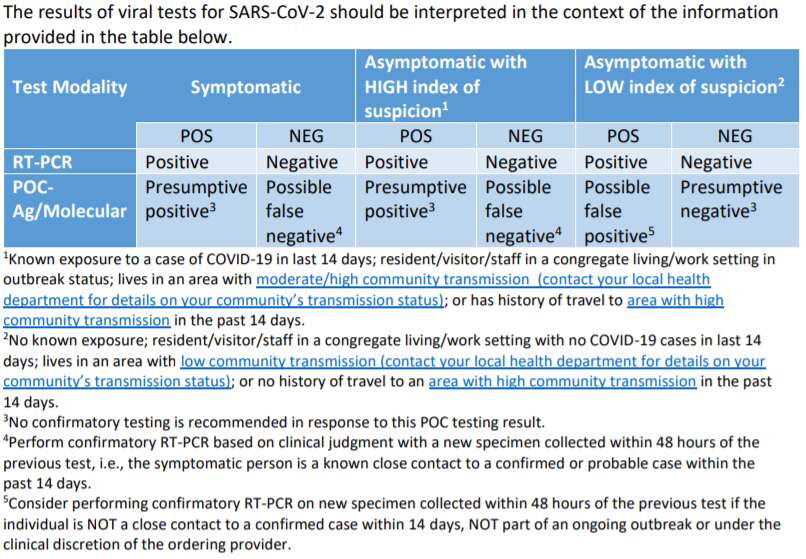
The most accurate, “gold standard” test for clinical diagnostic detection of COVID-19 (SARS-CoV-2) is Real-Time Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) more commonly known as “PCR testing”. Other tests are available and include rapid point-of-care (POC) molecular test and the POC antigen tests. POC tests, commonly known as “rapid tests,” have a higher probability of missing an active infection and it may be necessary to confirm rapid negative test results with a PCR test.
When might it be necessary to confirm a negative rapid test result with a PCR test?
In certain instances, a negative test result in a rapid test should be followed up by a PCR test. For example, if the result of the rapid POC test is inconsistent with the patient’s symptoms. In other words, if a patient has active COVID symptoms but receives a negative result, that person should proceed to PCR testing.
There are other instances when it is recommended to proceed to PCR confirmation of a negative rapid test. For example, when you have been exposed to a known positive case for more than 15 minutes within 6 feet it is recommended to obtain testing. If your rapid test is negative, PCR confirmation would be best practice.
Given what we know about the decreased accuracy of rapid testing, what are the most appropriate uses for rapid testing?
Rapid testing is extremely useful when it is positive. However, it will not change the plan for the patient. Patients who are symptomatic and positive will be instructed to isolate for a minimum of 10 days from the onset of symptoms while they are contagious to others. Patients who are asymptomatic but have had a “close contact” exposure will be instructed to quarantine for 14 days from the date of exposure.
Rapid testing may be an appropriate test for those who have no symptoms and no exposure. For example, some people are required to obtain a negative COVID-19 test prior to travel.
Roots Health DPC is committed to providing accurate COVID-19 testing information to you and your loved ones.
There are many different tests being offered with a constantly changing landscape of locations and availability. We understand that this can be overwhelming. It is our hope that this resource can help you navigate what type of test is best for you and your loved ones. Wherever you choose to test, please makes sure you know what type of test is being offered and have your questions answered before testing.
At Roots Health DPC, we currently offer PCR testing with a return time of 48-72 hours. All persons who test with Roots Health DPC are provided relevant and clear CDC recommendations including information on what to do while waiting for your test result, understanding the difference between quarantine and isolation, understanding how to manage COVID-19 symptoms at home, and learning how best to prevent the spread in your home if you have COVID-19.
If we can be of service or answer any questions, please feel free to reach out to us directly at 708-613-7916.
>>Click here to schedule a COVID-19 test<<
>>LEARN MORE ABOUT ROOTS HEALTH DPC<<